Can you try and define pain? Pretend you are explaining it to someone who has never heard about or felt pain…… Pretty tricky isn’t it. Well, you are not alone. The definition for pain has changed several times over the years.
Currently the international association for the study of pain (IASP) defines pain as an “unpleasant sensory and emotional experience associated with actual or potential tissue damage!”
It’s important to remember that each individuals’ pain is unique to them. We cannot feel it. But this doesn’t mean it’s not real!
Have you ever noticed a little kid fall over and scrape their knee? Their first reaction is to look for their parents for support. That is usually followed by tears until Mum/Dad give it the magic rub and say “it’s all okay.” 5 mins later and that kid is running around again with no care in the world. But, shouldn’t their knee still be sore?
After running around in the park all day this same kid gets home and asks for an egg sandwich. Mum fires up the cook top as she leaves the room. The poor kid decides he doesn’t want to wait, grabs the hot pan and burns himself. I bet they won’t be doing that again any time soon. Pain has taught this kid that the hot pan is not too be touched!!
Pain is a protective response and can help change our behaviours for the good and unfortunately for the worst.
Pain is also complicated.
So, what is pain?
Perhaps our simplistic way of thinking about pain has created some of the major issues’ society is currently dealing with. Pain is the most common reason people seek medical help. 1 in 5 Aussies currently are living with pain and this figure jumps to 1 in 3 people over the age of 65. Watch out, this number is expected to rise due to Australia’s ageing population. The estimated cost of pain in 2007 was a whopping $34 billion 🙁 and this number has most certainly grown since that date.
Got your attention? Cool – bear with me for a quick science run down of what pain actually is.
So, imagine you break your leg – sensors in the nerve around the tissue open to allow messages to be sent. (the amount of sensors change depending on what is needed – you get better at delivering these danger messages the longer you have pain) This message is then sent to spinal cord where it acts like a little brain processing the information. (again, the spinal cord can change and become more sensitive to the danger message). This message is then sent to the brain where it communicates with all of the brain tissue to come up with a conclusion for this message. This means language, vision, beliefs, fear, memory, movement, planning of tasks, other stress responses, etc. all help to deliver the output of pain. But the brain can also decide to reduce the pain intensity by producing hormones such as adrenaline to allow this poor person the opportunity to get to the hospital to get medical help.
So, what have we learnt;
Pain is an output from the brain
There are no pain sensors just danger ones
Humans are bioplastic and our bodies are constantly changing
Pain relies on context
We now also know pain can be influenced by stress (cortisol hormone changes), sleep (CNS sensitivity), immune responses (why we ache when we are sick).
For this very complicated danger response we have come up with a simple solution – PAIN KILLERS! (why do we even call them Pain Killers??) Some of us love them, some avoid them. But is it really that black and white? Can something be both good and bad?
Opioids or pain killers slow down messages between the brain and the rest of the body. They also help release dopamine which leads to sensations of pleasure and pain relief. This has helped millions of people suffering with acute pain. But are opioids beneficial for someone who is suffering with chronic pain? They estimate that 1% of the total burden of illness to society is actually caused by opioid use.
Let’s rewind back to the gentleman who broke his leg. In hospital the medical team will be giving him pain silencers (my new word for opioids) to help reduce the intensity of the pain during this acute stage. This is good as it allows the man to become medically stable and is discharged from hospital with a pain prescription. We know it takes ~6 weeks for bones to heal so thus we expect his pain to improve gradually with the tissue healing. However, this man has been taking the pain silencers for 6 weeks and still has pain?? Where to next? Do we increase the dosage?
Tissue damage doesn’t equal pain
Unfortunately, this is a common scenario and by increasing the dosage the gentleman becomes more dependent on the drugs which can lead to an overdose. They have also linked long term opioid use to increased pain levels in people with chronic pain. Long term opioid use has also been linked to mental health issues which we know can really influence someone’s pain response. Can you see the terrible loop that we have fallen into?
This table best describes what has happened to the gentleman;
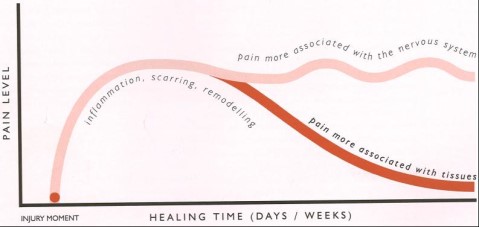
He is experiencing pain despite tissue healing. This is related to the changes in the nervous system
So how do we help this man? First off, we educate him about what the pain killers are doing to his body. We educate and discuss with him his fears about his pain. We try and help him understand the painful response that he is going through. And we explain;
It’s okay to hurt
If we stopped every time something hurt we wouldn’t accomplish much as a society. We gradually expose this gentleman to the painful tasks and over time this gets easier and easier. We introduce exercises and give this gentleman control of his life again. He gets stronger and stronger (bones, muscles, tendons etc). His mood improves, he is sleeping better, eating better, worrying less. Slowly but steadily we have flicked the switch from danger to safety and his pain slowly settles 🙂
Wow – and guess what that is just the tip of the iceberg! I could go on and on for pages and pages but I do not have time. I have to go and help people get themselves out of pain 🙂
If you know anyone who is experiencing pain please encourage them to take control of their lives again and book a consultation with a physiotherapist to discuss and create a rehab plan tailored for them.
You don’t have to live in agony any longer – sort out your pain.
If you would like further information on this forever changing beast please check out Lorimer Moseley’s Ted Talk ‘Explain pain’. He is a Pian Scientist but started his professional life as a Physiotherapist He has done a lot of research to disprove our common beliefs about pain. He has a unique story that he shares about his own experience with pain. He was running in the bush and was bitten by a snake which didn’t hurt and almost cost him his life. But the next time he was running in the bush and felt a scratch it was the worst pain he has ever felt!
Thank you body for trying to protect us!
by – James Wotherspoon, Physio